Abstract
Background: Results of conventional therapy in patients with peripheral T-cell lymphoma (PTCL) are dismal. Current guidelines recommend consolidation with autoSCT after 6 course of induction for most PTCL patients, but one third of new diagnosed patients progressed before autoSCT. Allogeneic hematopoietic stem cell transplantation (alloSCT) can cure relapsed/refractory patients, even those failured to HDT/ASCT. We hypothesized that AlloSCT as first-line consolidation post short course of induction could improve outcome in high-risk PTCL patients.
Patients and Methods:
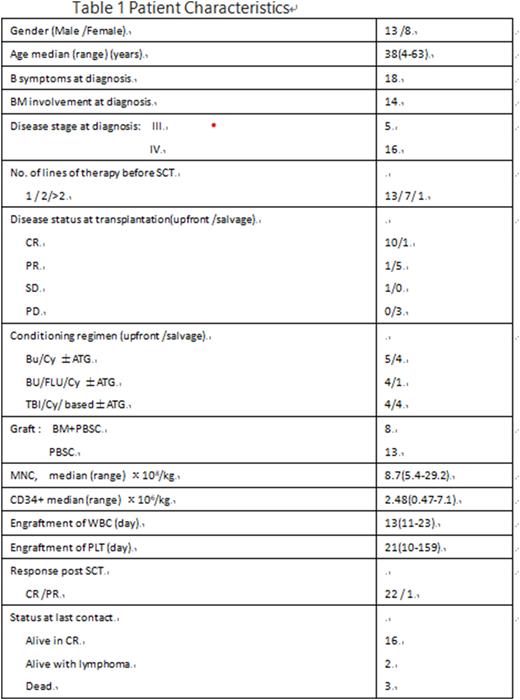
A prospective study was conducted in high-risk PTCL patients (except ALK+ ALCL, and stage 1 with aaIPI 0) who were scheduled to undergo upfront allo-SCT after 3 x CHOEP(or -like) induction chemotherapy (registered in Clinical Trials, NCT03672084). Matched sibling donor(MSD) was the first choice, an unrelated donor or haploidentical family donor(Haplo-donor) search was performed in patients without MSD. From Jan.2018 to June 2022, 23 newly diagnosed patients enrolled, 8 PTCL-NOS, 1 ALK-negative ALCL, 6 AITL and 9 HSTL. After 1st line induction, 12 proceeded upfront alloSCT(10 in CR,1 in PR and 1 in SD), 9 of 11 with progressive disease received transplant after 2nd line chemotherapy (salvage alloSCT), the other 2 (diagnosed with PTCL-NOS) did not undergo transplantation because of PD. All patients received myeloablative conditioning and antithymocyte globulin was administered for Haplo-SCT (with 2.5mg/kg daily on days -5 to -2). All patients received cyclosporineA, MMF and short-term MTX as GVHD prophylaxis (Patients characters were in Table 1).
Results: Untill July 30,2022,we had an interim results with the median follow up of 367(38-1237)d. For all transplanted patients, the median age was 38(4-63) years old, five had a MSD and the other 16 had a haplo-donor. Before alloSCT, 11 patients (52.4%) were in CR and 6 (28.6%) in PR, 1 (4.7%) in SD, and 3(14.3%) in PD. All but one patients had CR post alloSCT, 1 in PR received donor lymphocyte infusion(DLI) on D30 then had got CR on D60. One patient received a second alloSCT from another haplo-donor because of secondary graft failure. Acute GVHD of grade II-IV occurred in 9 of 21 patients (42.9%) (6 of grade III-IV). Thirteen of 20 (65%) evaluable patients developed chronic GVHD, which was extensive in 4 cases(20%). Four patients, all diagnosed with HSTL, experienced with post-SCT relapse on day 60,75, 180 and 455 respectively. Two had response to salvage chemotherapy with DLI, and stay in CR at last follow-up. Three patients died, 2 of lymphoma and 1 of pneumonia on day 280.
The estimated 1- and 2-year event-free survival (EFS) in all transplanted cases were 78% and 67%, and those of overall survival(OS) were all 83%. The D100 and 1-y toxicity-related mortality(TRM) were 0% and 6.4%, respectively. There were no differences in PFS and OS between upfront and salvage alloSCT. The patients who diagnosed with HSTL had a significant poor PFS compared to other types of PTCL, with the 1y PFS of 56% vs 92% (p=.017), and had a comparable 1-y OS ,78% vs 92% (p=.337). This result may due to the higher relapsed rate of HSTL (44% vs 0%, p=0.003). So we involved a prophylaxis DLI in HSTL patients recently.
Conclusions: Upfront AlloSCT in high-risk PTCLs was feasible with low TRM, and it could provide long-term disease control. And the strategy of haplo-donor SCT can bring more patients to AlloSCT. However, half of patients had progressed disease after 1st line induction, due to the strong anti-lymphoma effect of allograft, salvage alloSCT had been shown increased response rate in this group of refractory patients. The treatment strategy of short-term induction followed by alloSCT may improve the outcome for high-risk PTCL patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal